In last month’s letter, I wrote about pain thresholds and how it impacts decision-making, which inspired us to create the MyAdvo Self-Advocacy Framework—our first “AdvoKit” now available in the new Resources Center! We wanted to illustrate how to adopt an advocacy mindset when navigating healthcare (and personally, I needed a reminder as I prep for my well-woman exam).
This month, I want to touch on pain further. In light of the CDC’s new guidelines recommending pain counseling before IUD insertions, I’ve been thinking a lot about why it’s taking so long for women’s pain to matter. Read on for how the Self-Advocacy Framework can help you ask your provider about pain counseling.
There are SO many common procedures painful for women. The ones we talk about regularly in the MyAdvo community are pap smears, colposcopies, IUDs, saline sonograms, HSGs, even transvaginal ultrasounds can be painful. And yet, here are some phrases we’ve all heard:
“It will be just a pinch.”
“It’ll be over before you know it.”
“You’ll just feel a bit of pressure.”
“You won’t feel it.”
“Just don’t think about it.”
“Pain is normal.”
We know these procedures are crucial for healthcare. Pap smears, for example, have reduced cervical cancer rates by more than half from the mid-1970s to the mid-2000s. So, why fix what’s not broken? Despite their effectiveness, cervical cancer is still the fourth most common type of cancer in the world, yet it’s also one of the most preventable when detected and treated early. In the US, about 30% of eligible women don’t get screened regularly. Although access is a main issue so is fear and anxiety of a pelvic exam or other gynecological procedures, leading to delay or avoidance. While pap smears are common, other procedures like IUD insertions can be even more painful and contribute to these fears.

What actually happens during an IUD Insertion?
This summer, we’ve had some breakthroughs on women’s pain:
The CDC recommended providers discuss pain management options with women undergoing IUD insertions
The FDA approved a self-collection HPV test as an alternate to the pap smear in May. They’re still reviewing at-home testing as a method, but it could gain approval by early next year.
IUDs are the second most popular form of birth control after birth control pills, with about 24.9% of women using them as a form of contraception. I also want to note that IUDs can be used as symptom management for endometriosis or fibroids. But the pain associated with IUDs is often overlooked, so much so that a TikTok trend emerged where women filmed themselves screaming in pain during the procedure.
What exactly happens during an IUD insertion? Here’s a breakdown (Source):
Speculum Insertion
Potential Pain/Discomfort: Insertion and expansion of speculum in vaginal area
Cervical Cleaning and (potential) Local Anesthesia
Potential Pain/Discomfort: Cool or wet sensation from antiseptic. If injection of local anesthesia used, stinging for pinching sensation in cervix.
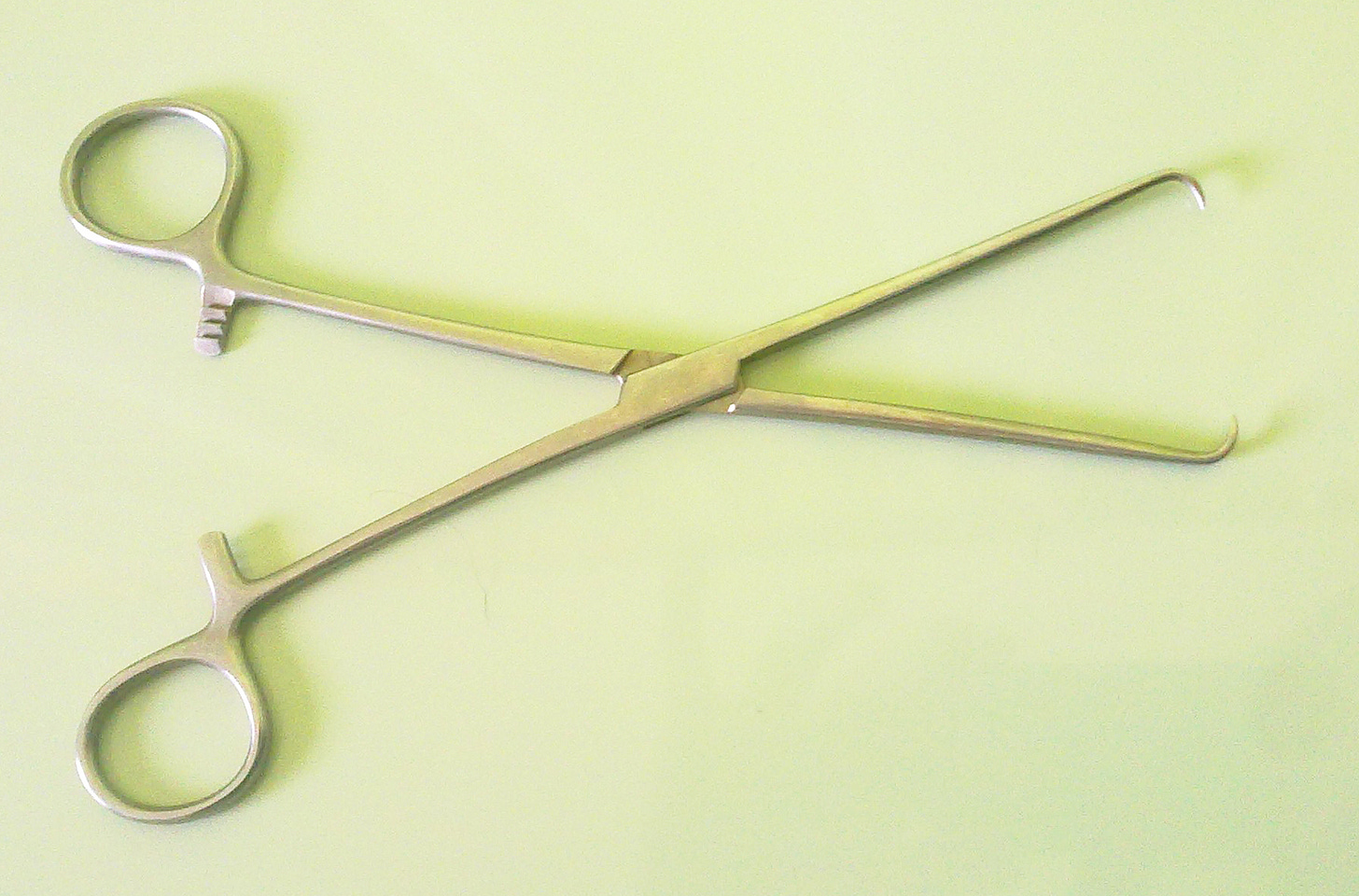
Cervical Stabilization: Tenaculum, a medical instrument that looks like a pair of scissors with hooks, may be used to grasp and stabilize the cervix to keep it steady during the procedure.
Potential Pain/Discomfort: Sharp, pinching pain or cramping from application of tenaculum to the cervix, which has sensitive nerve endings.
Measuring the Uterine Depth: A thin rod called a uterine sound is gently inserted through the cervix into the uterus to measure its depth and ensure correct placement of the IUD.
Potential Pain/Discomfort: Cramping as cervix and uterus may react to insertion of the sound by contracting.
Insertion of the IUD: The IUD, which is folded inside a plastic tube, is inserted through the cervix into the uterus. Once in place, the IUD is released from the tube, and the arms of the IUD open into its T-shape.
Potential Pain/Discomfort: Cramping or sharp, pinching pain as IUD passes through cervix and enters uterus.
Removal of Instruments: The insertion tube, tenaculum, and speculum are removed. The IUD strings are trimmed to an appropriate length.
Potential Pain/Discomfort: Mild cramping may continue as uterus adjusts to the presence of the IUD.
Post-Procedure Recovery
Potential Pain/Discomfort: Cramping or spotting can persist for a few hours to a few days after the procedure as the body adjusts to the IUD.
Look, everyone’s pain threshold is different. But I think you can agree, after reading these steps, that pain counseling is a minimum. When you don’t really know what the procedure entails, it’s hard to understand WHY it’s SO painful when you’re told “it’s just a pinch.” (ahem…have you seen what a tenaculum looks like?)
What does good pain counseling look like?
As much as providers aren’t to blame for medieval-looking instruments and poor pain management options, women do (again, at a minimum) deserve pain counseling.
As patients, it’s asking providers about pain management options and determining if they’re the right fit for us. For providers, it’s reciprocating with education on what happens during a procedure, why it’s necessary, and why they think it’s the best choice for their patient. At the very least, acknowledging that pain may occur allows for a conversation about the patient’s pain threshold.
A MyAdvo community member with endometriosis went through the exercise when she discovered she may have a blocked fallopian tube after reviewing her medical records from a surgery over 5 years ago (story for another time…). She made an appointment with her Fertility Specialist, and we worked through the Self-Advocacy Framework together:
Set your goal(s):
She’s thinking of conceiving next year.
She prefers to minimize the use of synthetic hormones if IVF is needed to avoid potential endometriosis regrowth.
Her main concern is timing pregnancy with her endometriosis pain after the IUD is removed.
Question everything: If she only has 30min, what’s the one thing she wants to get out of her appointment?
Is testing required separately or can they recommend undergoing the procedure to fix the fallopian tube based on her medical records?
What testing (if any) confirms a blocked fallopian tube? What’s the least painful option given her endometriosis?
Ask for help: Her Fertility Specialist recommended FemVue—a saline sonogram—versus an HSG that uses contrast dye to help with pain management.
She pinged her support groups to see if other women had experienced FemVue and to understand how to prep.
Weigh options: She discussed with her partner when to do the testing as part of their larger plan to conceive.
Act: She established a timeline based on her other health concerns to space out testing and procedures, knowing many of these will be painful.
The CDC's pain counseling recommendation is a step in the right direction, but we need effective pain relief. Even lidocaine, used for procedures involving the cervix and uterus, can fall short. Both patients and doctors agree: more research is urgently needed because providers are working from a limited toolbox.
So what’s holding us back?
IMO it comes down to lived experience and funding. Men can’t feel women’s pain, so it’s often not a priority.
We’ve needed to pass laws for women to be prioritized in medicine.
Historically, women were treated as “small men.” Women’s bodies were considered the same as men’s except smaller and with reproductive organs. Medicine formed around male physiology, the assumption being, that if women weren’t responding the same way, then it had to do with our psychology rather than our biology. Women have been excluded from medical and science knowledge for most of history. Our hormones introduced too many variables in clinical trials (aka made them too expensive and complicated). It wasn’t until 1993 that the NIH and FDA mandated including women and minorities in clinical trials via the Revitalization Act (just another reminder of how important it is to stay tuned to policy and vote for who you want representing you and your health). Sadly, a 2022 study found that women are still underrepresented in clinical trials for leading diseases.

This brings me to my second point on why the needle hasn’t moved: the gender wealth gap. This isn’t just how much women make compared to men but rather how much they have—cash, investments, real estate, minus debts. Women own 32 cents for every dollar a white man has. With less wealth, women have less to invest in. And what does research need? Funding.
I know this can all feel oppressive, but I’m a believer that you can make a difference by just speaking up—with your girlfriends, family, partner, and especially at your doctor’s office. Take a look at our Self-Advocacy Framework, and let me know if it helps next time you head to the doctor’s.
MyAdvo Monthly Reads
(policy, podcasts, research, trends & more to advocate for yourself)
🥇 Olympian Brittany Brown talks about her endometriosis
📚 Disordered eating is more common in PCOS, regardless of body weight
💊 Women in England to be offered a daily tablet for fibroids
⚖️ Texas hospitals wouldn’t treat ectopic pregnancies due to abortion law
⚖️ EPA issues emergency order to stop use of a pesticide harmful to fetuses
⚖️ Chinese court overrules single woman’s appeal to freeze her eggs
👩🔬 NIH launches $3 million prize competition to modernize diagnosis of endometriosis




